
The Standard
for Clinical
Breast Exam
The Breast Exam Training and Practice Network, created and supported by the MammaCare Foundation, measurably improves and validates essential clinical breast exam skills worldwide.
MammaCare has trained more than 9,000 providers in 11 countries on 5 continents with our first-in-class training technology powered by the cloud.
The Breast Exam Training and Practice Network, created and supported by the MammaCare Foundation, measurably improves and validates essential clinical breast exam skills worldwide.
MammaCare has trained more than 9,000 providers in 11 countries on 5 continents with our first-in-class training technology powered by the cloud.
Lifelike breast cancers detected
Breast exams performed
1,200+
Certifications
Join the Network

Clinical Breast Examiner Certification
Trains and certifies performance of clinical breast exams onsite via teletraining technology.
Certification is valid for 3 years.
Health Departments
Breast Clinics

AI Breast Exam Trainer
Trains your students and staff to perform proficient clinical breast exams using MammaCare's web-based AI Breast Exam Trainer.
Training curriculum intended for
Universities
Health Departments
Breast Clinics
VA Health

CBE Standards & Practices Course
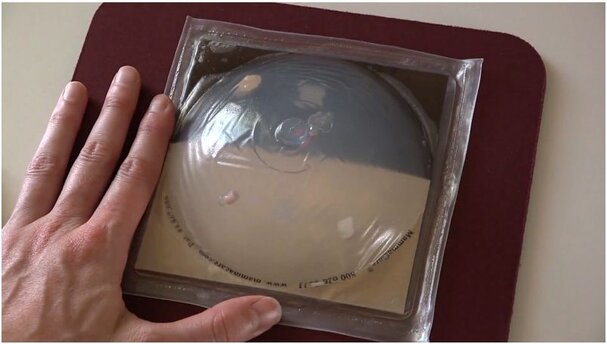
Teaches and validates breast exam skills on transparent and opaque breast models containing suspicious lumps.
Training curriculum intended for
Universities
Breast Clinics

Essential Palpation Course
Allows your students to see what they are feeling as they are introduced to clinical breast exam skills and important breast health topics.
Training curriculum intended for
Universities

Breast Self-Exam Instructor Certification
Trains and certifies educators to teach women to perform breast self-exams in their communities through group workshops.
Certification is valid for 3 years.
Training curriculum intended for
Breast Clinics
Educators
Health Departments




Breast Self-Exam Instructor Certification
Become certified to teach women to perform breast self-exams in your community through group workshops.

The MammaCare® Foundation is a 501(c)(3) non-profit dedicated to training every hand that examines a woman, including her own. The MammaCare Method is the recognized standard for performing and teaching clinical and personal breast examination. MammaCare provides clinical certification services and high-fidelity simulation-based training.
Phone
+1 352 375 0607
Address
930 NW 8th Ave,
Gainesville, FL, 32601
United States


